Can Red Light Support Testosterone & Testicular Health?
Jan 05, 2026
image: Luminouslabs Pro Series 2.0
Hormonal health in men is often discussed in terms of numbers — testosterone levels, lab ranges, and quick interventions. What is discussed far less is why hormone production declines in the first place and what actually supports long-term testicular function.
Photobiomodulation (PBM), commonly referred to as red or near-infrared light therapy, has been studied for its effects on inflammation, cellular energy, and tissue recovery. More recently, research has begun exploring its role in testicular health, testosterone production, and male fertility.
This blog explains what the science shows, how light interacts with testicular tissue, and why photobiomodulation is best understood as a supportive biological tool, not a shortcut.
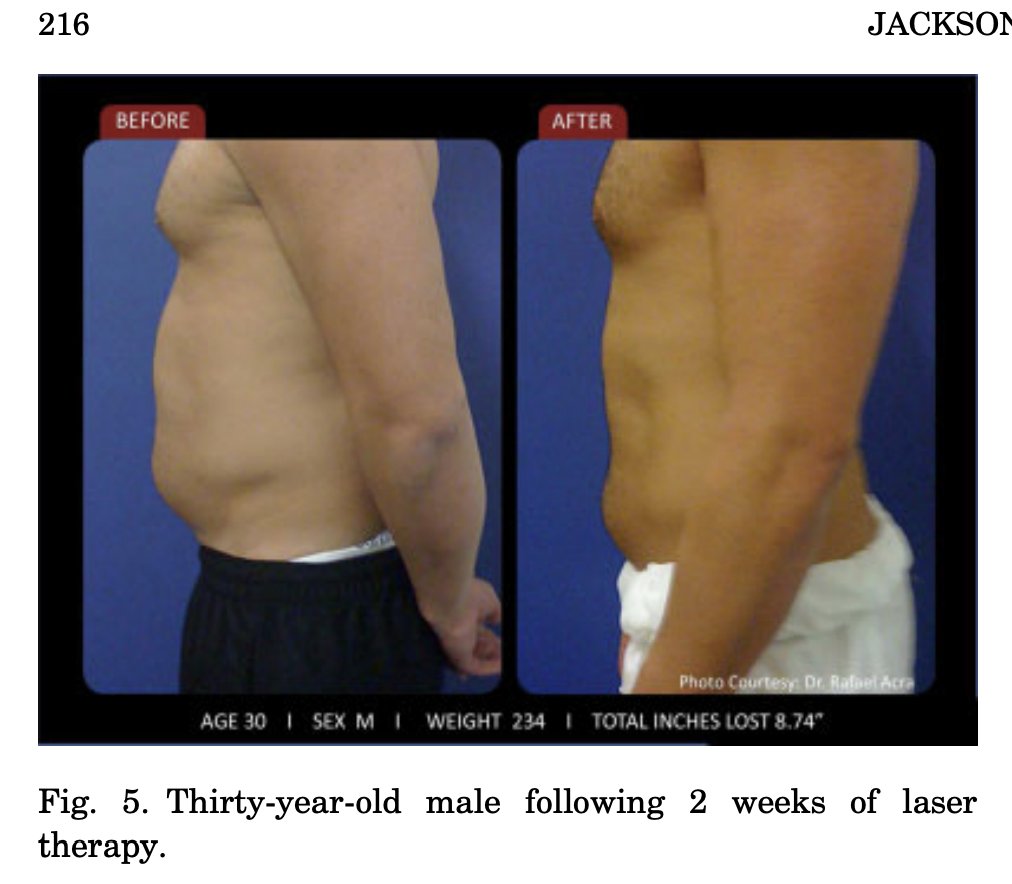
Light does this. From gut problems, to low T and even fat loss. Why light may just be the missing link to enhance your metabolism:
Testosterone Depends on Tissue Health, Not Stimulation
Testosterone production occurs in Leydig cells within the testes. These cells are highly energy-dependent and sensitive to inflammation, oxidative stress, and disrupted blood flow.
Several animal studies examining testicular dysfunction caused by spinal cord injury or chemical suppression show that when near-infrared light is applied locally, testosterone levels increase and move closer to normal physiological ranges. Importantly, this effect reflects functional recovery, not forced hormone production.
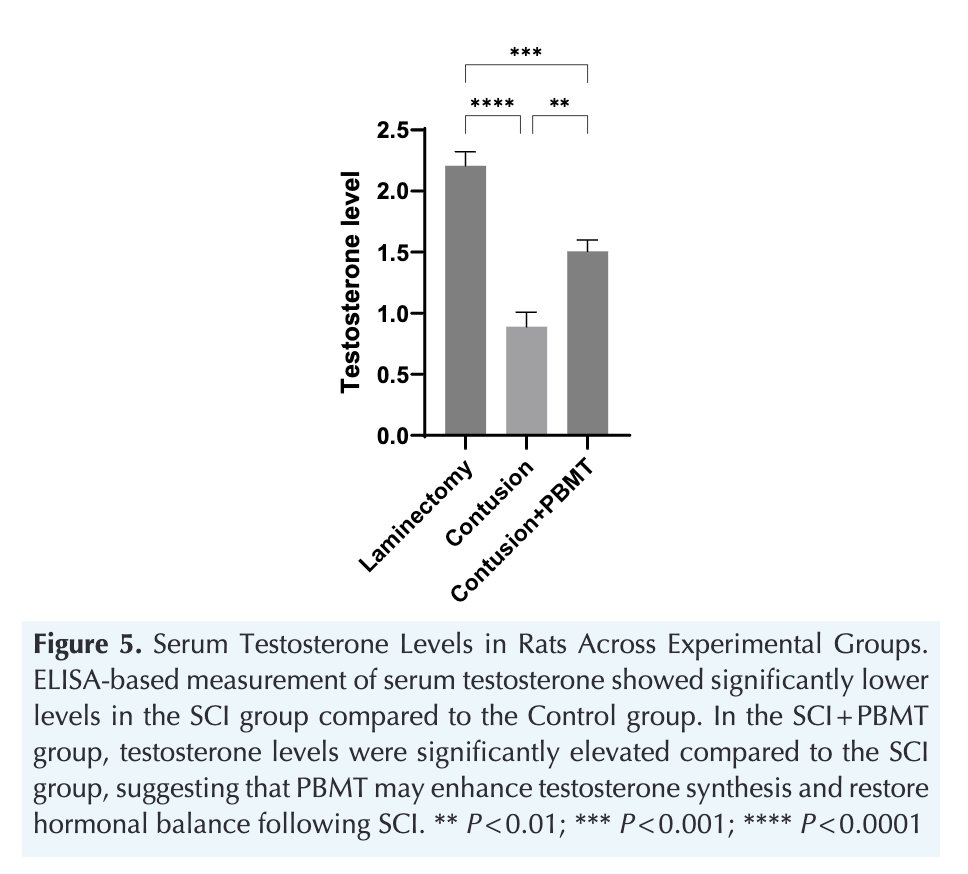
The light increased testosterone at 810 nm.
Photobiomodulation does not override endocrine regulation. It supports the cellular environment that allows hormone synthesis to occur naturally.
Testicular Structure and Volume Can Recover After Injury
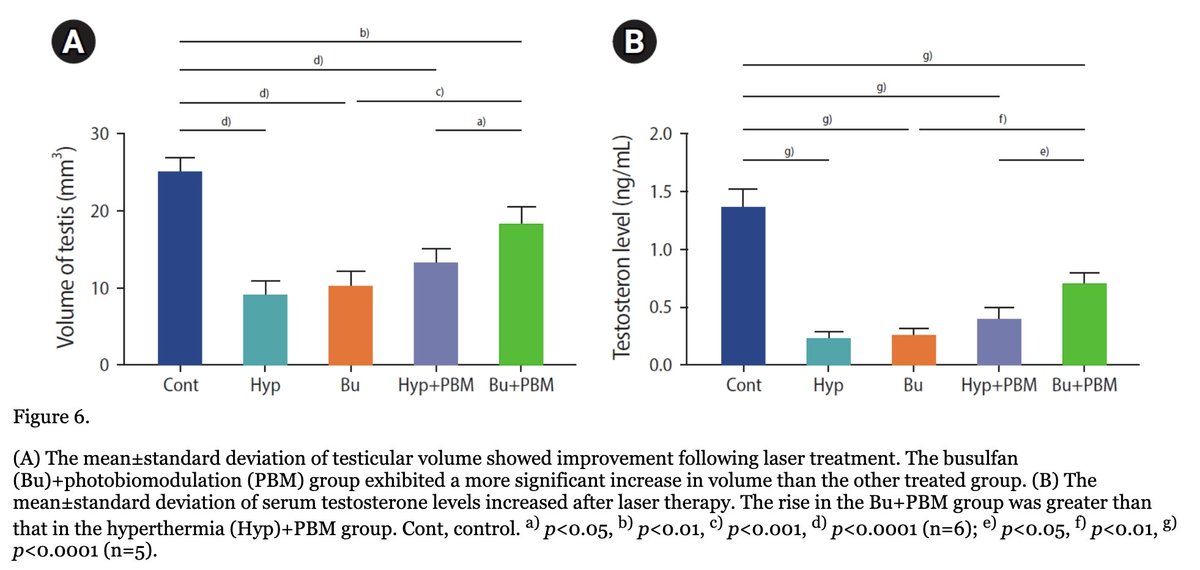
In models where testicular tissue was damaged chemically, near-infrared light exposure was associated with increases in both testicular volume and testosterone output.
This suggests that light therapy supports tissue integrity and endocrine capacity. Structural recovery matters because hormone production cannot occur in damaged or atrophied tissue, regardless of external stimulation.
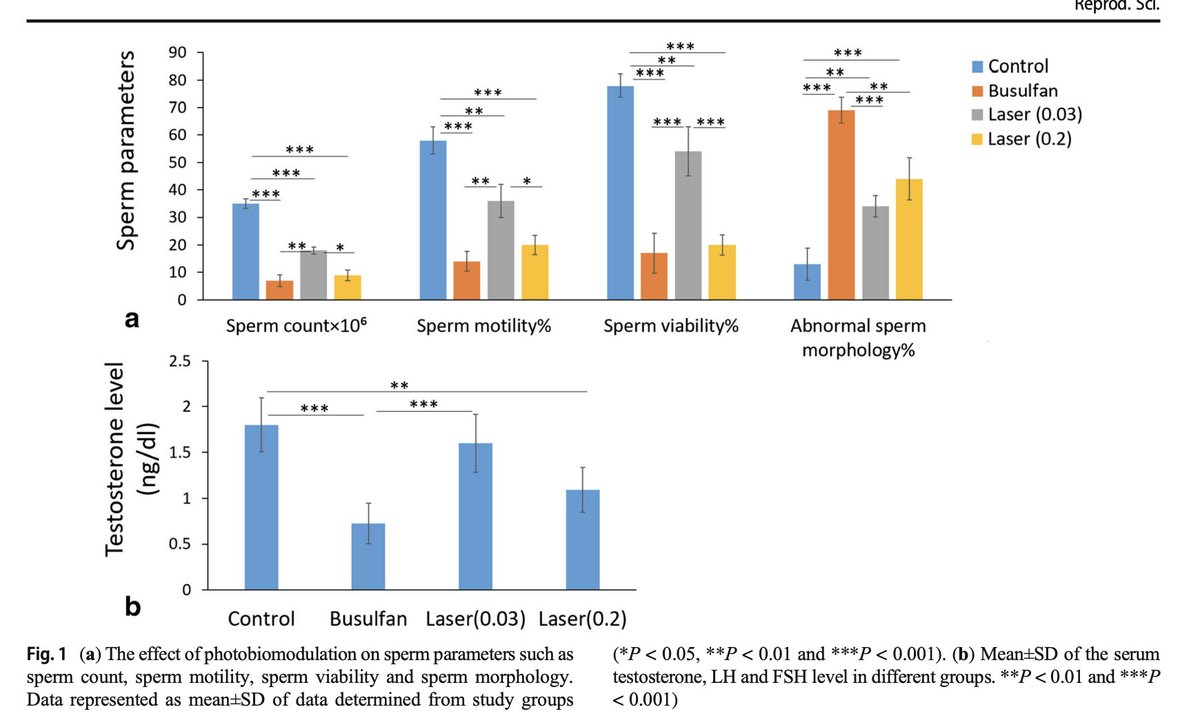
Fertility Markers Improve Alongside Hormonal Recovery
Hormonal health is only one aspect of male reproductive function. Across multiple studies, photobiomodulation improved key markers of sperm health, including:
-
sperm count
-
motility
-
viability
-
morphology
These findings indicate that light therapy supports spermatogenesis, not just circulating hormone levels. When the testes regain structural and cellular integrity, fertility markers tend to improve alongside testosterone.
Inflammation Is Reduced Inside Testicular Tissue
Chronic inflammation is a well-recognized contributor to low testosterone and impaired fertility. Pro-inflammatory cytokines such as TNF-α and IL-1β disrupt Leydig and Sertoli cell function and damage spermatogenic tissue.
Photobiomodulation has been shown to significantly reduce these inflammatory signals while increasing anti-inflammatory activity within the testes. This shift creates an internal environment more compatible with hormone production and tissue repair.
Cell Death Is Reduced, Preserving Hormone-Producing Cells
Healthy testosterone production depends on the survival of Leydig and Sertoli cells. Excessive apoptosis (programmed cell death) reduces the testes’ capacity to produce hormones and support sperm development.
Markers of apoptosis, including caspase-3, are reduced following red or near-infrared light exposure. Fewer cells are lost, allowing tissue function to be maintained over time.

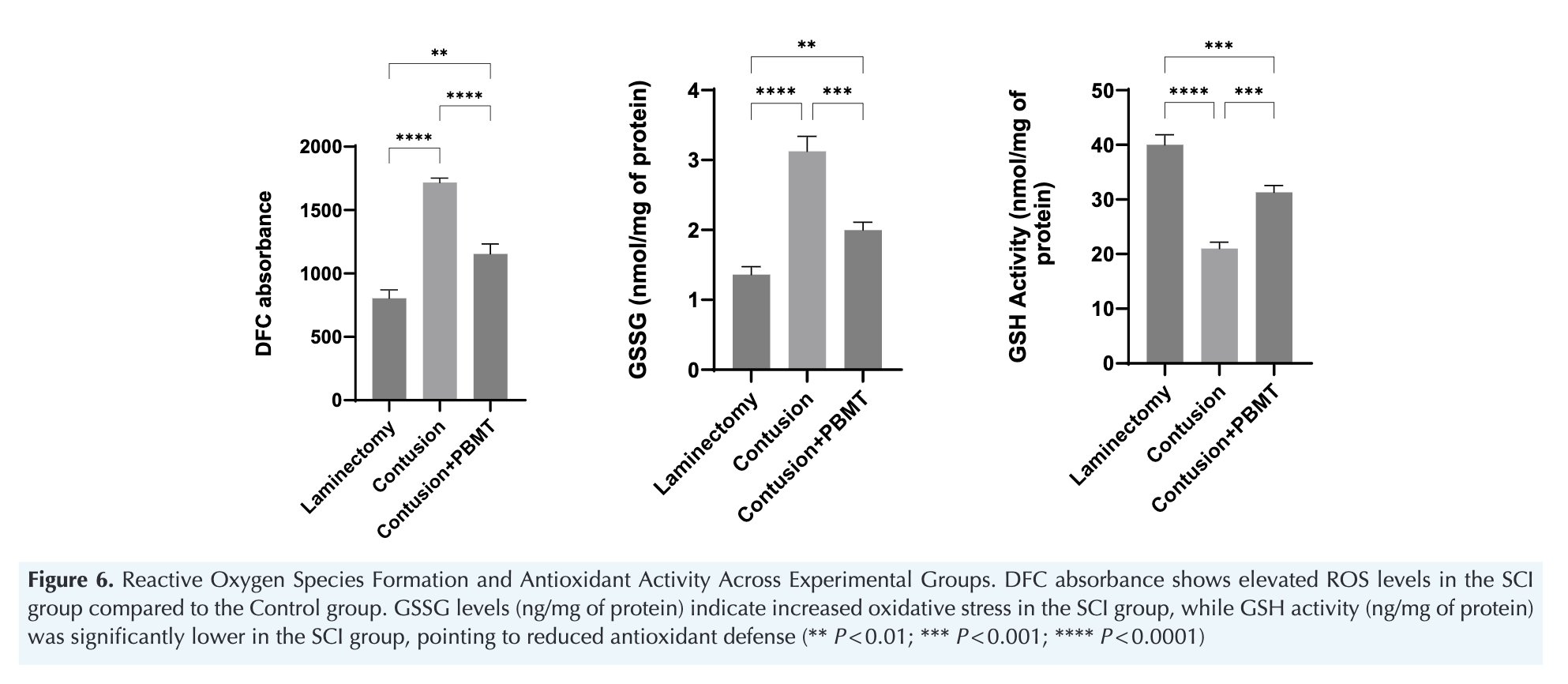
Oxidative Stress Is Lowered and Antioxidant Balance Restored
Oxidative stress directly impairs steroidogenic enzyme activity and damages mitochondrial function. When reactive oxygen species overwhelm antioxidant defenses, testosterone synthesis declines.
Photobiomodulation reduces free radical production and improves the glutathione balance (higher usable GSH relative to GSSG). This improved redox state supports mitochondrial efficiency and restores the biochemical conditions required for steroidogenesis.
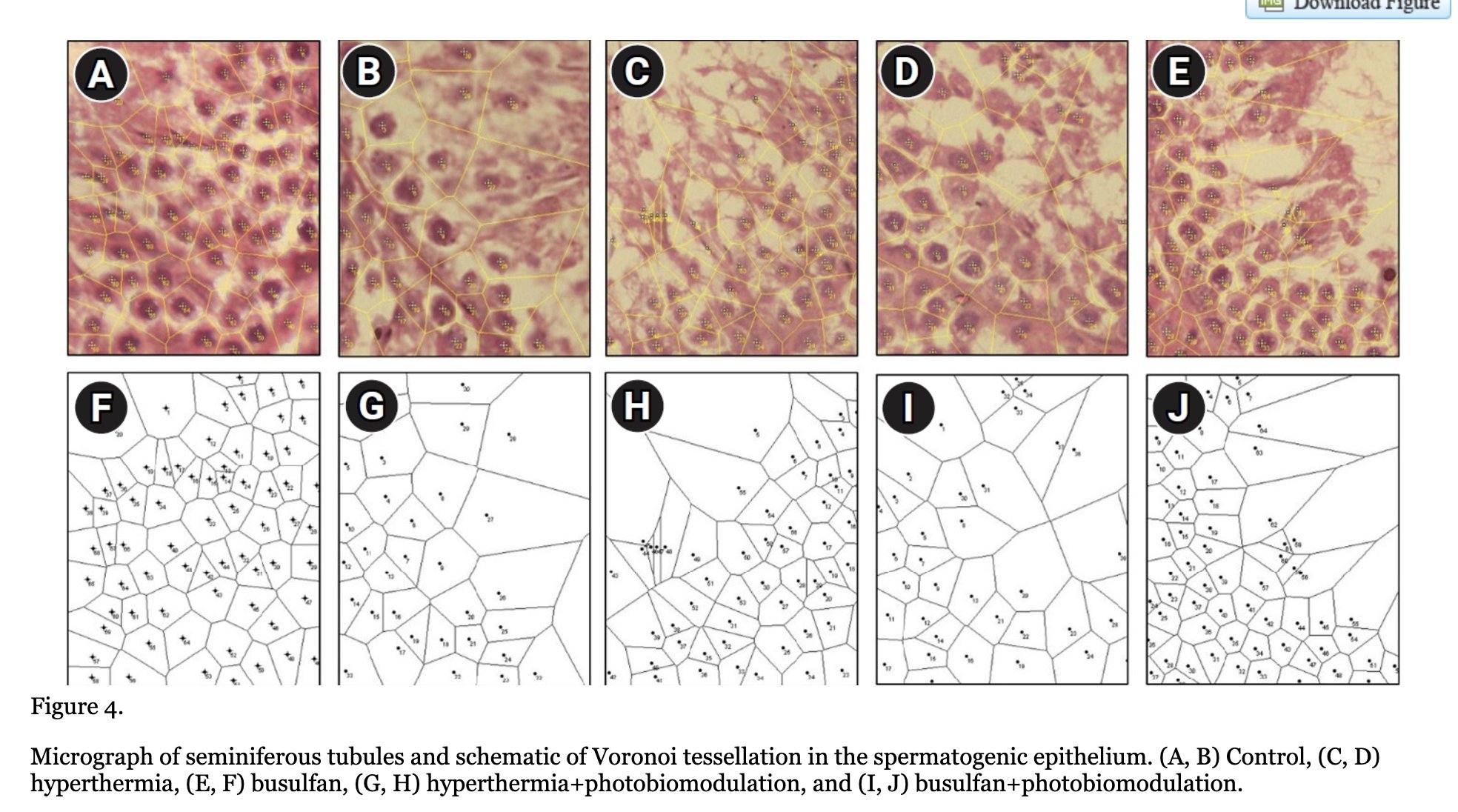
Structural Recovery of Seminiferous Tubules
Microscopic examination of testicular tissue shows that photobiomodulation improves the structure of the seminiferous tubules, the site of sperm production. Improved organization, cellular density, and tissue integrity confirm that the effects of light therapy are not limited to blood markers — they occur at the tissue level.
Function follows structure. When tissue integrity improves, reproductive capacity improves with it.
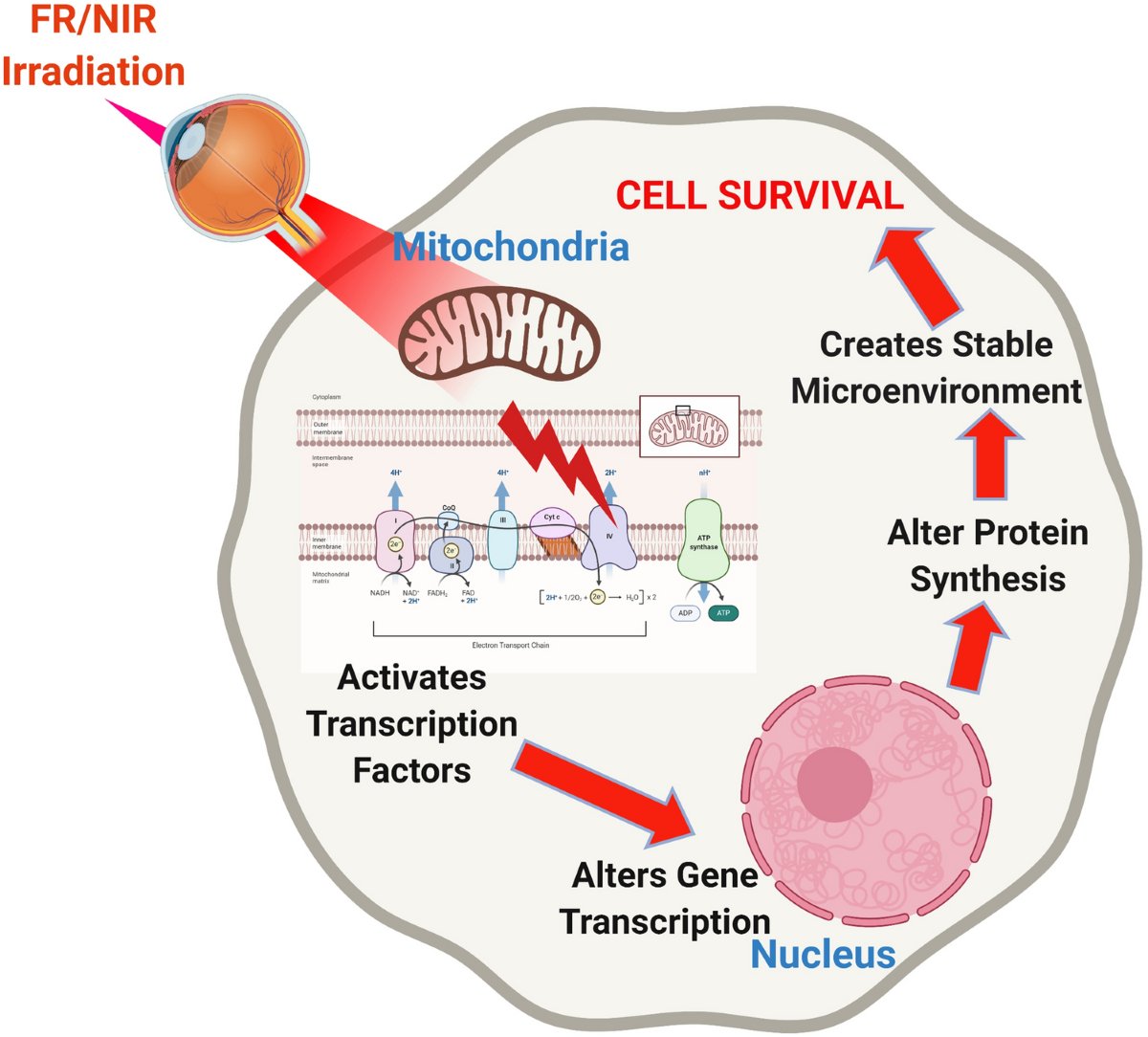
The Central Mechanism: Mitochondrial Energy
So how does red and near-infrared light exert these effects?
The primary mechanism begins at the level of the mitochondria, the organelles responsible for cellular energy production.
Specific wavelengths of red and near-infrared light interact with a key mitochondrial enzyme, cytochrome c oxidase, within the electron transport chain. When this enzyme is stimulated, mitochondrial efficiency improves.
As a result:
-
cellular ATP production increases
-
excess free radical generation decreases
-
the balance between NAD⁺ and NADH shifts toward a healthier redox state
All three are essential for cellular resilience and tissue function.
The reduction in free radical burden has additional downstream effects:
-
gene expression and intracellular signaling become more favorable
-
cellular damage is limited
-
inflammatory signaling is dampened
This is particularly important for Leydig cells, which are highly sensitive to oxidative stress and are responsible for testosterone production.
A significant proportion of low testosterone and impaired fertility is driven not by hormonal failure, but by chronic oxidative stress and inflammation within testicular tissue. When that environment improves, cellular function can recover.
Red light does not “switch on” testosterone.
It supports the energetic and biochemical conditions that allow testosterone production to occur naturally.
This is why photobiomodulation acts upstream — at the level where biology actually operates.
What This Means for Men
Photobiomodulation is not a replacement for sleep, nutrition, movement, or stress regulation. It is best understood as a supportive intervention when systems are under strain due to chronic stress, inflammation, metabolic dysfunction, or recovery from injury or illness.
Used appropriately, light therapy can help restore the biological conditions required for hormonal and reproductive health.
Final Thoughts: Why Light Matters for Male Health
Male hormonal health is not driven by willpower, supplements, or shortcuts. It is the result of cellular energy, tissue integrity, blood flow, and inflammatory balance.
Photobiomodulation does not “boost” testosterone artificially. It supports the biological environment required for testosterone and sperm production to function properly. By improving mitochondrial efficiency, reducing oxidative stress, lowering inflammation, and preserving hormone-producing cells, light therapy helps restore capacity rather than force output.
The takeaway is simple:
testosterone is not something to chase — it is something the body produces when the conditions are right.
Photobiomodulation helps improve those conditions.
Practical Application & Device Considerations
Understanding the biology is only one part of the equation. For photobiomodulation to be effective, how it is applied matters.
For smaller, localized tissue areas, red and near-infrared light therapy is typically used in short, consistent sessions rather than prolonged exposure. The goal is to stimulate cellular signaling and mitochondrial function without overwhelming the tissue.
In practice, we generally recommend:
-
10–15 minutes per session
-
Once daily, or at least 3–5 times per week
-
Applied directly to the target area, following manufacturer-recommended distance guidelines
Consistency matters more than intensity. Photobiomodulation works through cumulative cellular signaling, not single exposures.
When clients ask which type of device we typically recommend for small, targeted applications, we look for systems that deliver both red and near-infrared wavelengths capable of penetrating tissue to reach the cellular level.
For this reason, we often point toward Luminous Labs Essential device for localized use, as their devices provide multiple bioactive wavelengths designed to support mitochondrial function.
 image: Luminouslabs Essential device
image: Luminouslabs Essential device
As with any therapeutic tool, red light therapy works best when integrated into a broader health strategy. Devices do not replace fundamentals — they support them.
References
pubmed.ncbi.nlm.nih.gov/40330513/
pubmed.ncbi.nlm.nih.gov/40351155/
pubmed.ncbi.nlm.nih.gov/39450003/
pubmed.ncbi.nlm.nih.gov/33825170/
Related blogs:
16 Proven Benefits of Red Light Therapy for Better Health, Wellness and Longevity
Choosing the Right Red Light Therapy Device: What to Look For and Why It Matters